
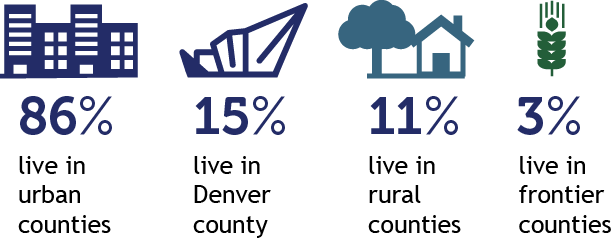
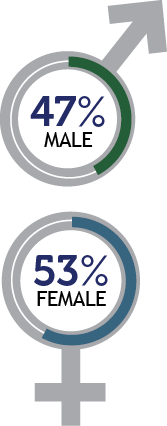
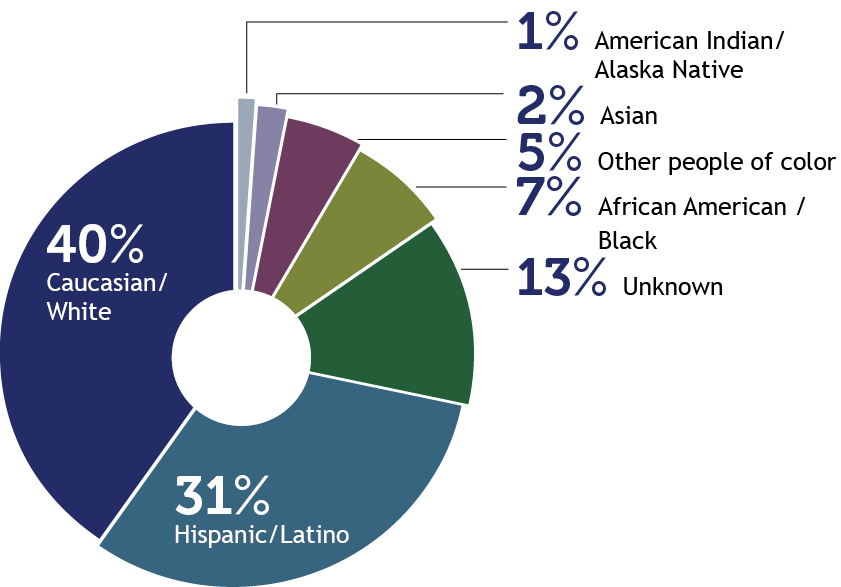
 Due to rounding, percentages may not total 100%.
Due to rounding, percentages may not total 100%.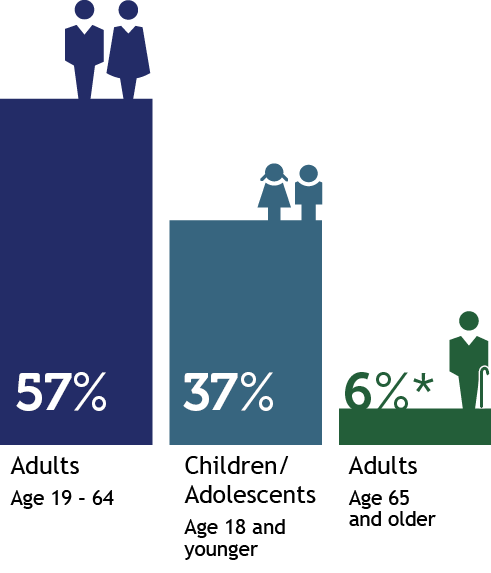
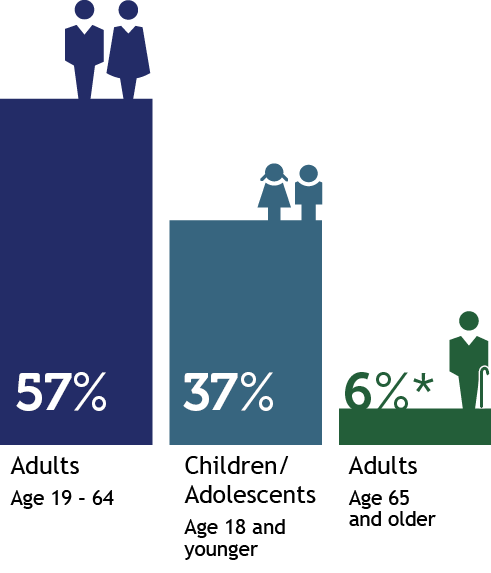
*Adults age 65 and older includes people partially eligible for Health First Colorado.

The Department administers Health First Colorado (Colorado’s Medicaid program), Child Health Plan Plus (CHP+), and other public health care programs for Coloradans who qualify.
Our mission is to improve health care equity, access and outcomes for the people we serve while saving Coloradans money on health care and driving value for Colorado.
 |  | ||
 |  Due to rounding, percentages may not total 100%. Due to rounding, percentages may not total 100%. | ||
 *Adults age 65 and older includes people partially eligible for Health First Colorado. |  | ||
 | |||
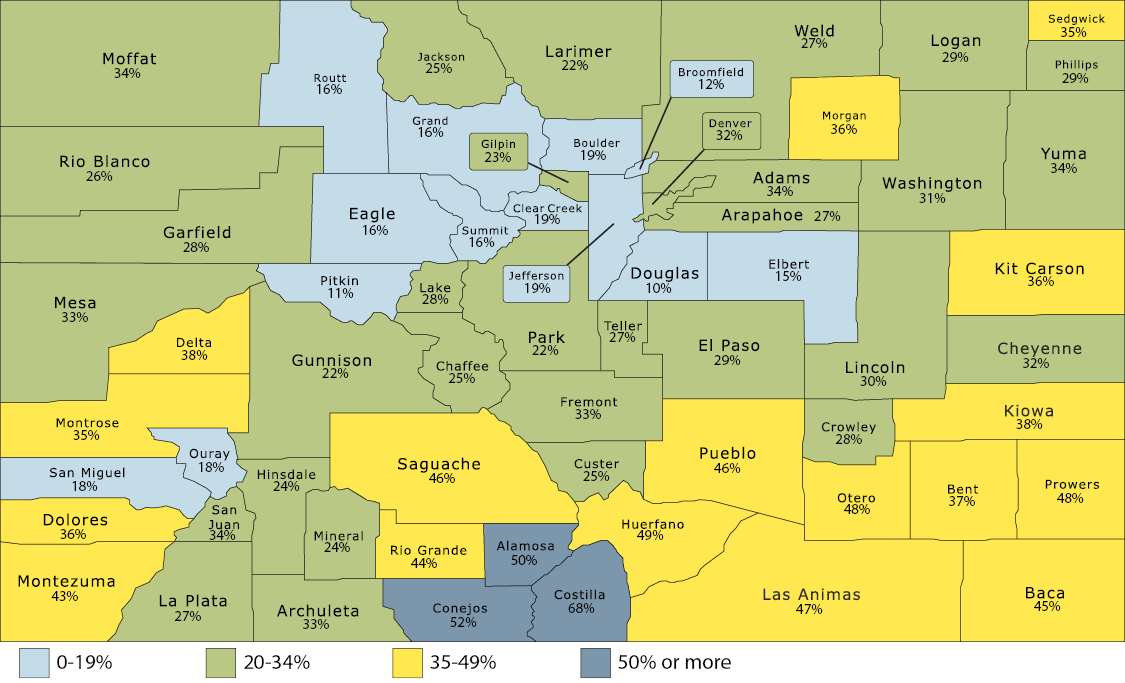
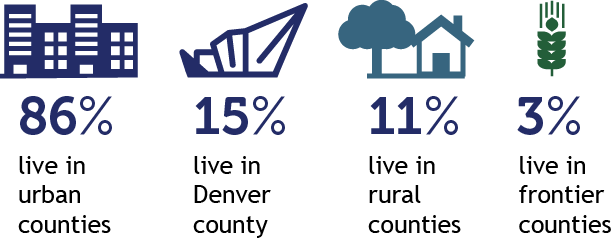
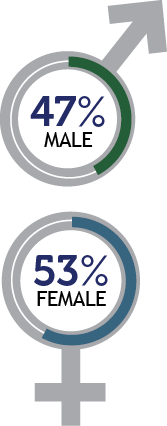
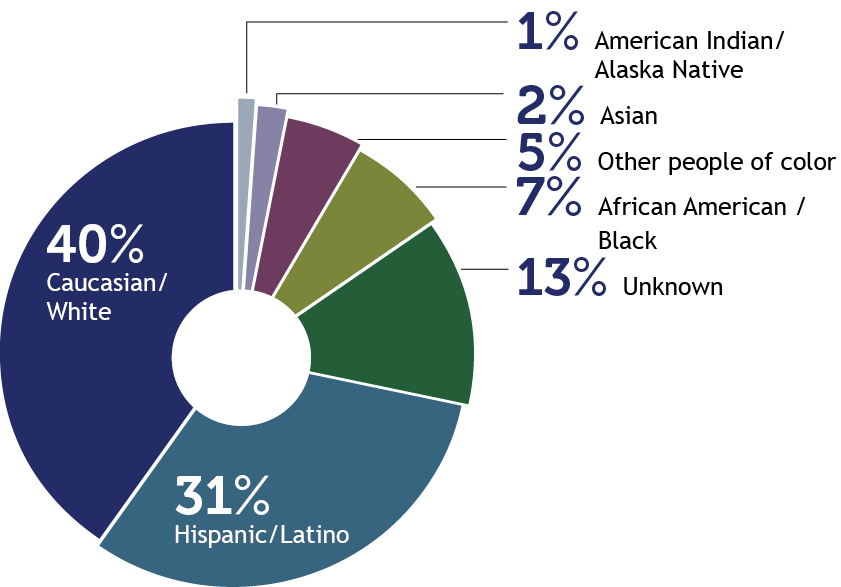
Source of enrollment data is Medicaid Management Information System (MMIS). Percentages represent people enrolled for one day or more during calendar year 2021. 2021 population data as forecasted by the state demographer.
1.6 M
members
Health First Colorado
Colorado's Medicaid program
A public health care program that provides access to physical & behavioral health care, hospitalization, nursing facility care, prescription drugs, dental care & other benefits.
![]()
53,000
members
Child Health Plan Plus (CHP+)
CHP+ provides comprehensive health care benefits, including dental care, to uninsured children ages and cannot afford private health insurance.
![]()
35,000
served
Colorado Indigent Care Program
CICP allows Coloradans with incomes up to 250% of the Federal Poverty Level to receive discounted health care services at participating hospitals, community health centers and clinics.
![]()
511,620
served
Dental Programs
Health First Colorado offers dental benefits to children and adults. The adult dental program completed its sixth year of services on June 30, 2021.
![]()
15,424
served
Buy-In Programs
The Health First Colorado Buy-In programs allow members with disabilities to pay a premium for Health First Colorado if they earn too much to qualify, so they don’t have to choose between work and health coverage. Learn more about Buy-In programs for adults and children.
![]()
62,510
served
Long-Term Services & Supports (LTSS)
| LTSS provides comprehensive care for members 65 and older and people with disabilities, so they can:

Live in a setting they choose with the supports they need

Participate in communities that value their contributions

Access services in a simple, timely & streamlined manner

Get the highest quality services
The Accountable Care Collaborative (ACC) is at the core of Health First Colorado. Launched in 2011, it creates Regional Accountable Entities (RAEs) that deliver the programs that will improve member health and reduce costs across the state. Learn more about the ACC.
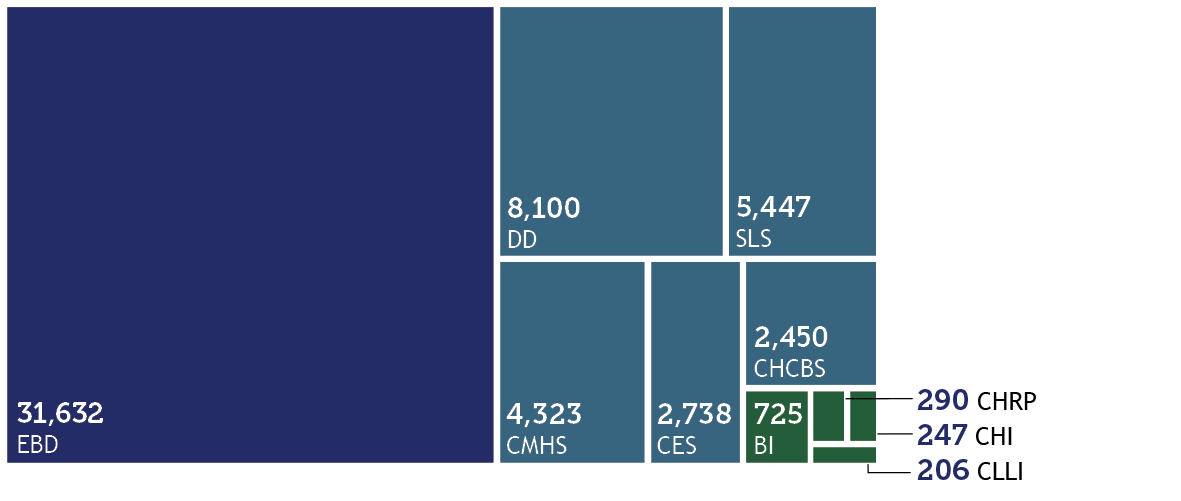
Elderly, Blind, and Disabled (EBD), Developmental Disabilities (DD), Supported Living Services (SLS), Community Mental Health Services (CMHS), Children’s Extensive Support (CES), Children’s Home & Community-Based Services (CHCBS), Brain Injury (BI), Children’s Habilitation Residential Program (CHRP), Complementary and Integrative Health (CHI, formerly known as the Spinal Cord Injury (SCI) waiver), Children With Life Limiting Illness (CLLI)
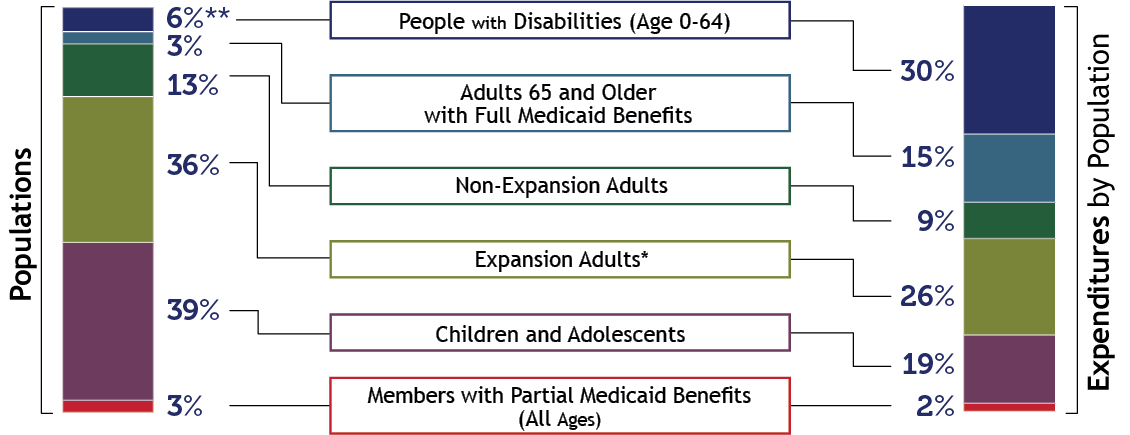
Patient Protection and Affordable Care Act (ACA) Medicaid Expansion. Due to rounding, percentages may not total 100%. *The majority of funding for Expansion Adults is federal dollars, with the state fund source funded by the Healthcare Affordability and Sustainability Fee.
**Not all members with disabilities use long-term services and supports.
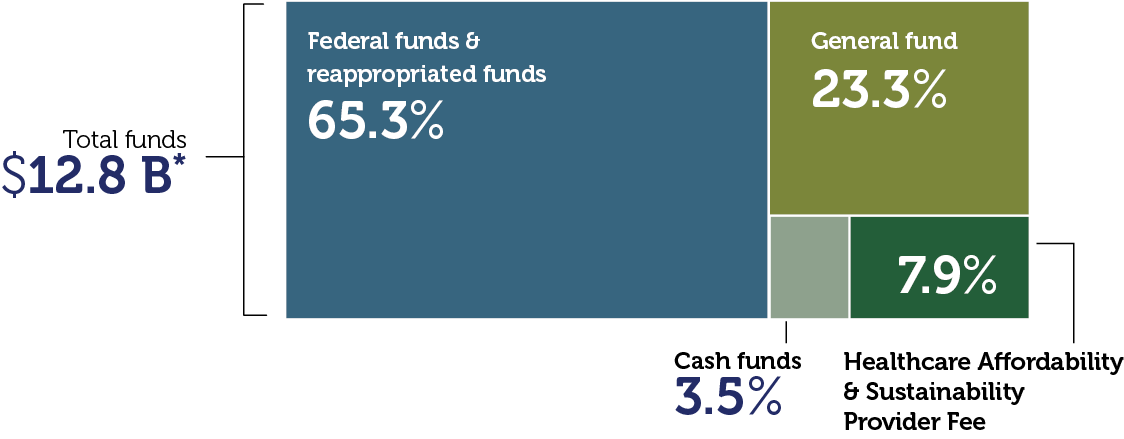
*Includes all services and administrative line items, including Colorado Indigent Care Program and Old Age Pension.
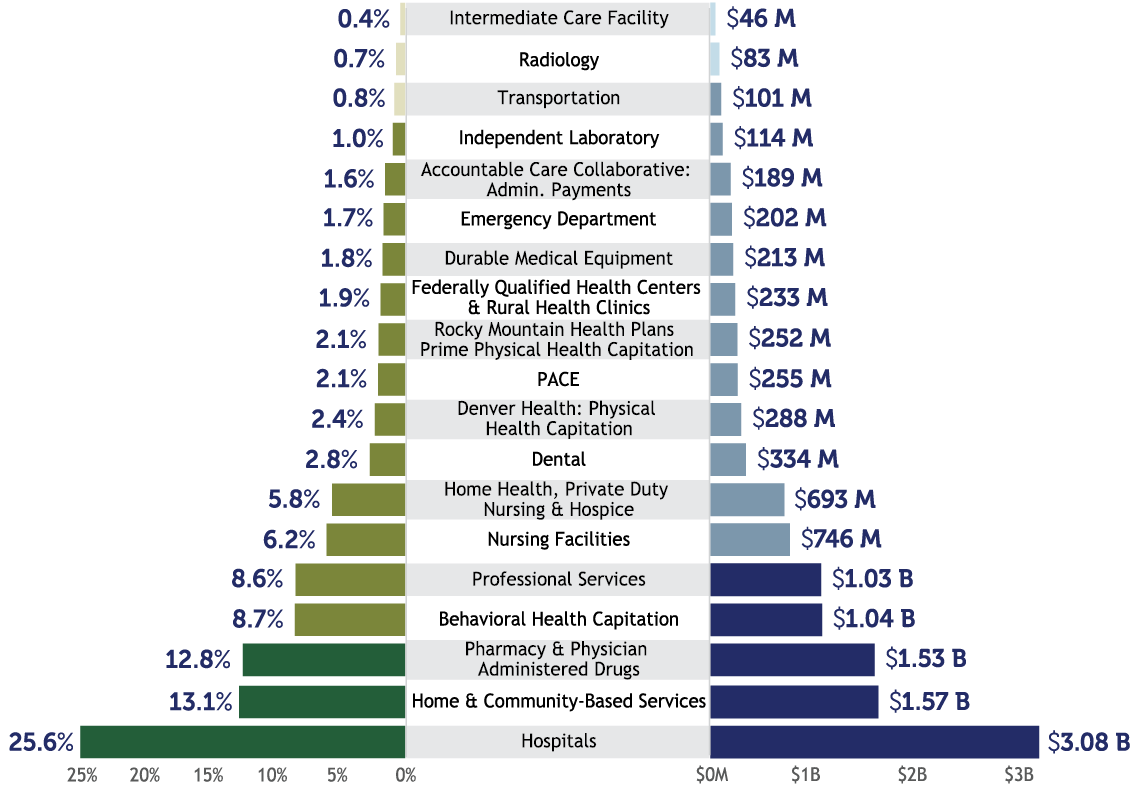
This chart refers to medical services cost only, not total Department spending. It is based on claims data by date of service and will differ from data calculated on a cash accounting basis. Due to rounding, percentages may not total 100%.
To support our mission, we focused on several priority areas:
| Transforming home & community-based care We received state and federal approval to leverage $530 million of American Rescue Plan Act (ARPA) federal stimulus to implement lasting transformation for people with disabilities and long-term care needs. Our initiatives enhance, expand and strengthen home and community-based services (HCBS) in Colorado through the end of 2024. There are currently 63 projects in progress to support recipients of long-term services and supports (LTSS), their families, providers and the health care workforce. Our most recent quarterly reports are available on our website. | Transforming behavioral health Thanks to General Assembly support of transformative legislation, the Department is partnering with the new Behavioral Health Administration to expand behavioral health services for our members. This includes adding residential beds, expanding the provider network, improving transparency and reporting, and catalyzing care coordination. To support this work, the Department has increased our investment in behavioral health by $400 million since FY 2018-19, now totaling over $1 billion annually, and has expanded the provider network to include 10,300 active behavioral health providers, including 1,000 added from September 2021 through August 2022. |
| Expanding the health care workforce The Department is part of a multi-agency state effort, with providers, advocates, members, families and workers, to expand and support the health care workforce. The General Assembly approved Health First Colorado rate increases for providers and certain health care workers, including a $15/hr minimum for direct care workers and those working in nursing facilities. The Department is investing in telemedicine, expanding data infrastructure, supporting the existing workforce, partnering on training, recruitment, and career pathway creation and helping identify geographic differences in the health care workforce. | Leading on affordability The Department is working to save people money on health care, focused on the top two drivers of health care costs: prescription drugs and hospital prices. To bring down prescription drug costs, the Department has made progress on value-based contracts and payments, drug importation where federally permitted, and the Prescriber Tool, driving to implement the affordability recommendations in our report: Reducing Prescription Drug Costs in Colorado. To make hospital services more affordable, the Department is partnering with hospitals to recognize where we are outliers in the nation, asking hospitals to make meaningful pricing changes. As part of that effort, the Department published nationally leading hospital price, cost and profit transparency reporting. Value-based payments are being implemented across the spectrum of care — hospital care, primary care, maternity care, behavioral health, prescription drugs and more — to reward quality outcomes and affordability. |
| Committing to health equity We updated our mission in 2021 to highlight our commitment to “improve health care equity, access and outcomes for the people we serve while saving Coloradans money on health care and driving value for Colorado.” While the Department is working hard to apply a health equity lens across all our programs and initiatives, we have identified four initial health disparity areas of focus within Health First Colorado, including: vaccination rates, maternal care, behavioral health and prevention. Read more about this in our first Health Equity Plan. | Ensuring continuous coverage At the beginning of the COVID-19 pandemic, the federal government declared a public health emergency (PHE) which required states to continue Health First Colorado coverage, even if someone becomes ineligible, among other things. Health First Colorado and CHP+ grew by more than 440,000 members (35%) and now serve 1.69 million Coloradans. That’s 1 in 4 Coloradans. As a result, together, we kept the uninsured rate steady at about 6.6% through the pandemic. With the economy rebounding and the federal PHE expected to end, the Department has a 14-month plan to make sure that people who are eligible stay covered and those who aren’t can find reduced cost coverage on the Connect for Health Colorado marketplace. |
| Improving member & provider experience The members who participate in our programs are at the center of everything we do. We track several metrics to ensure we’re improving their experience and collect real-time feedback from our Member Experience Advisory Council. In the past year, our Member Call Center answered calls in less than 30 seconds on average. Eligibility system innovations and automation have driven our automatic approval rate to approximately 34% for all members renewing. This means there is no member or eligibility worker activity needed for these approvals. These system innovations have also enabled us to process 97% of applications within 45 days. For our providers, claims were processed in less than four days and calls were answered in well under one minute on average through the last half of the year. Together, we have handled the 35% membership growth without any major operational issues and expanded the Health First Colorado provider network by 28% over the past few years, with 96,800 providers now enrolled. | |
I am extremely proud of our accomplishments together over the past fiscal year (July 2021-June 2022), which is reflected in this annual report. Thank you for your partnership in another unprecedented year for health care. Together, we successfully served an additional 440,000 Coloradans in need — an increase of 35% — since the start of the pandemic.
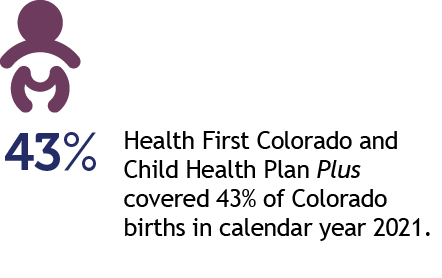
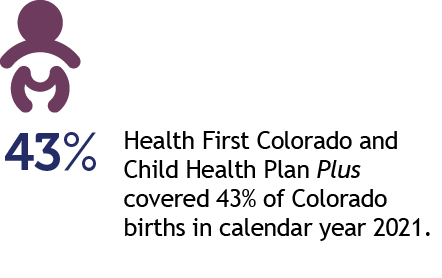
We are covering 1.69 million, or one in four, Coloradans — including more than 40% of Colorado’s children and more than 40% of births in the state.
This support during the pandemic has been a lifeline for Coloradans. Our safety net programs have helped keep Coloradans covered through the COVID-19-induced economic downturn, maintaining a steady 6.6% uninsured rate. This annual report shows how we not only grew our provider network to meet the needs of members, but also how we invested in health care delivery to improve care quality, service, equity and affordability. We appreciate our partners who worked with us through this pandemic. For more detailed information on what we accomplished together, please see our Performance Plan.
Looking ahead, there is still much work to do to help Coloradans thrive. We’re focusing our efforts on several key areas in the coming months.
Thank you again for your ongoing partnership in transforming health care for the betterment of our members and all Coloradans. I hope you enjoy this annual report.

Kim Bimestefer, Executive Director, HCPF